New cancer treatment tested in patients
Researchers at DTU can improve the immune system's T cells to attack cancer cells in certain melanoma patients. In collaboration with Herlev Hospital, the solution is now being tested in patients.
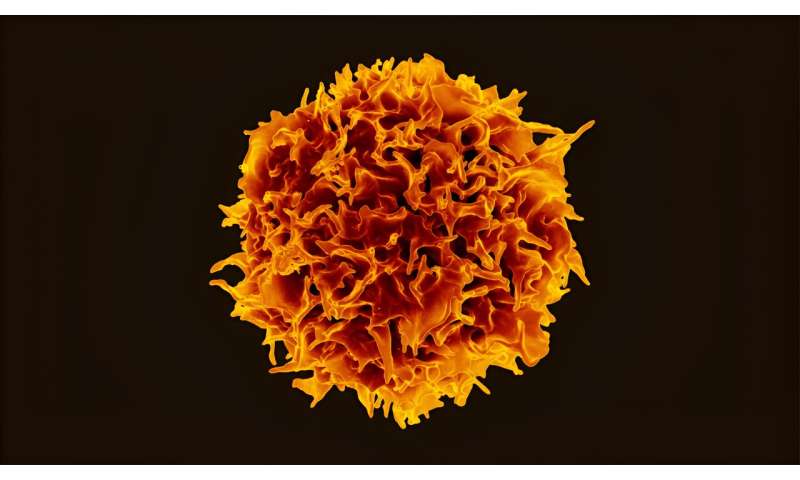
Professor Sine Reker Hadrup from DTU has been researching the use of T cells for cancer treatment for many years. T cells are a special type of white blood cells that play an important role in our immune system. Most recently, Professor Hadrup's research group has developed a method to boost the ability of T cells to recognize cancer cells and multiply them to form a massive cancer-fighting army.
Initially, this has been done in the laboratory based on small blood samples from patients, but the process is now ready for upscaling.
"We take a bag of blood from the patients, identify and multiply the T cells that are able to recognize antigens on the surface of cancer cells, and then return the cells to the patients," explains Hadrup.
The procedures have been refined, and the substances used to engineer the T cells have been quality-assured. And just over a year ago, everything was ready to start an actual clinical trial at Herlev Hospital.
First target is melanoma
Initially, the trial comprised patients with advanced melanoma who had undergone several standard treatments without significant improvement. Only patients with tissue type HLA-A2 were eligible, which goes for approximately 40% of all people in Europe. And a third selection criterion was that the patient's blood should already contain a small amount of the type of T cells that are able to tackle cancer cells.
So far, five patients have received this treatment.
"It's a very small trial, which was primarily intended to show something about the safety of the treatment. We're only now starting to analyze all the data, but fortunately we can see that there have been no side-effects. We also need to make sure that the cells we give back to patients actually stay in the body. But most importantly, we hope to see a reduction in tumor size in some of the patients," says Hadrup.
Plan to include more cancers
Alongside this clinical trial, Professor Hadrup and her team are still working to further develop and refine the technology.
"We're looking at other cancers where the technology might be relevant. More specifically, we've worked with one of the rarer forms of skin cancer, Merkel cell carcinoma, which is virus-driven. We have previously characterized which sequences from this virus the immune system's T cells are able to recognize. Therefore, we can now create a library of sequences that we know are relevant, and then we can mix and match them depending on the patient's tissue type. This will enable us to make products that can be used on a larger sample of patients—at least 90% of all tissue types. It works in the laboratory, and we hope to soon be able to start a clinical trial," says Hadrup.
One of the major challenges associated with T cell technology is that it is a heavy process involving a lot of logistics and requiring access to advanced laboratories such as cleanrooms, and processing of the blood cells of individual patients. So it is unrealistic for it to become the standard treatment for wider patient populations.
"However, working with the technology improves our understanding of the immune system, and we would like to use our knowledge to create new off-the-shelf technologies. We're moving towards not working with patients' own cells, but generating cells from stem cell lines or donors with a matching tissue type, which can then be kept in the freezer until needed. It means that more patients will be able to benefit, and we will be able to eliminate the waiting time from when a decision is made to offer T cell therapy until the actual treatment can start. The normal production phase is often several weeks," says Hadrup.
Nanoparticles are coming
A newer research track is opening up even greater perspectives. Together with another research group at DTU Health Tech, headed by Associate Professor Yi Sun, and Professor Hinrich Abken from Regensburg University Clinic, Hadrup's group is developing nanoparticles that, when injected into the patient, can find the T cells that need to be trained to fight the cancer cells.
The researchers will conjugate the nanoparticles with antibodies that allow them to be absorbed by T cells, and they will carry genetic information that enables the T cells to better recognize the cancer cells.
All treatments potentially come with side-effects; the researchers are very aware of this when building the nanoparticles. The components must not be toxic in themselves, and in so far as is possible they therefore choose components that have been used in other medical contexts, or which are similar to something known to be compatible with human tissue.
"Many other groups in the world are working to develop such particles, so a lot is happening in this field, and I'm convinced that it will be done within the next few years. Whether our particle will be the preferred one, time will tell. In any case, different strategies are needed to reach the T cells. They come in many versions, and different T cells are needed to target different cancers," says Sine Reker Hadrup.
Provided by Technical University of Denmark