Whipple procedure: a perspective on progress
This History Maker article was written by the coauthors in collaboration with Dr. John Cameron and is based on several detailed discussions with Dr. Cameron. The paper focuses on Dr. Cameron's leadership in the revolutionary improvement of surgical results for the Whipple procedure in the 1980s.
Today, many medical centers are achieving excellent results with the Whipple procedure, as documented in the USA and Europe. Dr. Cameron notes that there are also centers in China, Japan, and India that use high-volume and other clinical approaches to achieve excellent results in pancreatic surgery.
The Cameron legacy continues at Johns Hopkins with excellent, low postoperative mortality rates. Additionally, within the last 10 years, there has been another dramatic change, namely, the introduction of even less invasive surgical techniques, such as laparoscopic and robotic surgery, to perform the Whipple procedure.
The surgical treatment of periampullary tumors began in the late 19th century, with two pioneers performing the first operations on this type of cancer. In February 1898, Dr. William Steward Halsted performed the first successful resection of a periampullary tumor with re-anastomosis of the pancreatic and bile ducts. The patient was discharged from the hospital but died from jaundice secondary to cancer recurrence a few months later.
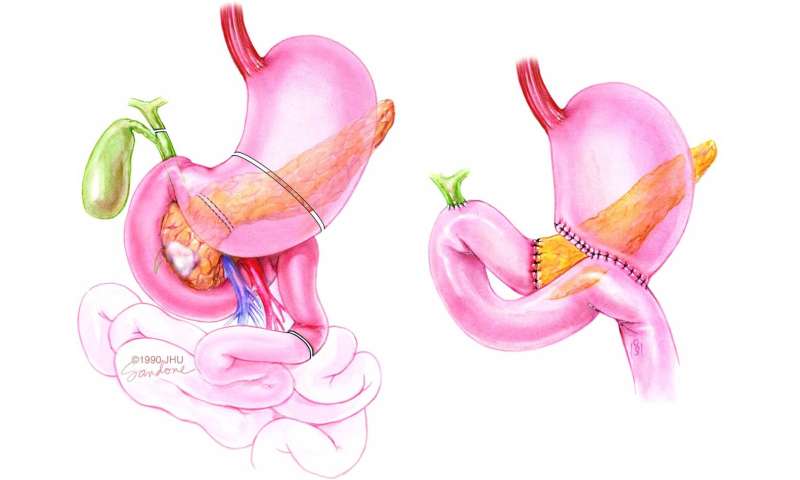
In 1909, Dr. Walther Kausch, in Germany, performed the first successful regional resection of the pancreatic head with pancreatic-duodenostomy. Dr. Allen Oldfather Whipple from New York published three cases in 1935 and popularized the modern standard techniques for pancreaticoduodenectomy, which later became known as the Whipple procedure.
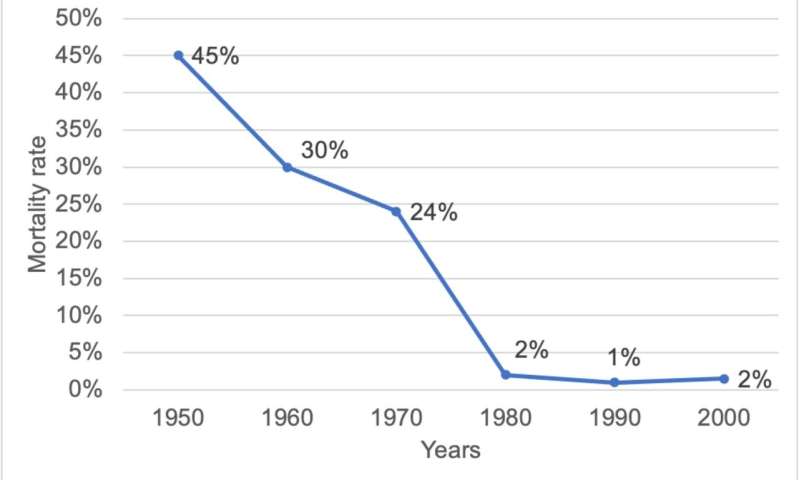
By 1963, Dr. Whipple had performed 37 pancreaticoduodenectomies. However, the Whipple procedure was nearly abandoned around this time due to a high in-hospital mortality rate of more than 25%. This high mortality rate was thought to be related to several factors, including:
- The lack of high-volume centers and surgeons
- The lack of well-established systems to address postoperative complications such as sepsis and hemorrhage
- Imprecise patient selection in the absence of advanced radiographic imaging
In the 1980s, there was a revolutionary transformation in pancreaticoduodenectomy, with high-volume centers (performing more than twenty-five cases per year) reducing in-hospital mortality to less than 5%. Dr. John Cameron of Johns Hopkins led this revolution, reporting a mortality rate of approximately 1%.
Dr. Cameron dedicated his career to improving pancreatic surgery. He performed over two thousand pancreaticoduodenectomies over five decades. He attributed his success to his adherence to Halstedian surgical techniques, which included gentle tissue handling, excellent hemostasis, careful dissection, and precise anastomosis.
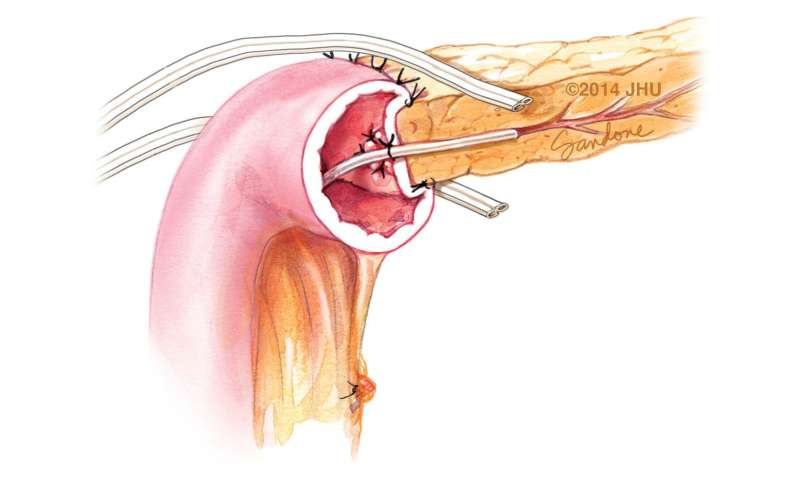
Dr. Cameron also made significant contributions to developing closed-suction drainage, which significantly reduced the sepsis associated with pancreatic leaks. He placed closed-suction drains right at the pancreatic-jejunal anastomosis, replacing the previously used Penrose and cigarette drains.
Dr. Cameron's work has profoundly impacted the field of pancreatic surgery. He is credited with leading the revolution that reduced in-hospital mortality for the Whipple procedure from over 25% to less than 5%. His adherence to Halstedian surgical techniques and his development of closed-suction drainage have made the Whipple procedure safer and more effective.
Dr. Cameron's contributions to pancreatic surgery are truly remarkable. His work has helped countless patients survive and thrive after pancreaticoduodenectomy. He is a true pioneer in the field, and his legacy will continue to benefit patients for generations to come.
More information:
Bo Chang Wu et al, Revolutionary transformation lowering the mortality of pancreaticoduodenectomy: a historical review, eGastroenterology (2023). DOI: 10.1136/egastro-2023-100014
Provided by First Hospital of Jilin University