Researchers develop a new CPAP device to assist with obstructive sleep apnea
An estimated 40 million adults in the United States have obstructive sleep apnea (OSA), a chronic sleep-related breathing disorder that involves a decrease or complete halt in airflow. Continuous positive airway pressure (or CPAP) is broadly considered first-line therapy for OSA.
CPAP technology is effective, but only if used regularly. Largely due to discomfort related to the mask and associated headgear required to maintain prescribed airway pressures by current devices, today's CPAP is not well tolerated by patients. Noncompliance is estimated to impact at least a third of patients according to 2016 research published in the Journal of Otolaryngology - Head & Neck Surgery.
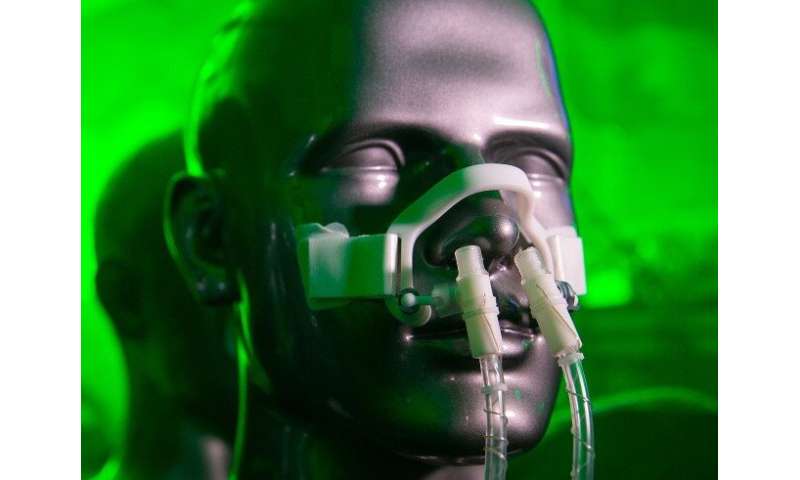
Researchers at the University of Cincinnati are developing a VortexPAP machine that takes advantage of vortex airflow technology. A preliminary clinical study with current CPAP users demonstrated that the VortexPAP can deliver the pressure levels that are used in the subjects' CPAP therapy, but the mask is more comfortable to wear. It has a minimalistic design that is less intrusive and barely touches the patient's face.
"Despite the clinical efficacy for CPAP in controlling OSA, patient compliance with the therapy remains a major cause of treatment failure," says Liran Oren, Ph.D., research associate professor in the Department of Otolaryngology, Head and Neck Surgery at the UC College of Medicine.
"The vast majority of complaints from patients in CPAP therapy revolve around improving the comfort of the mask," explains Oren. "However, regardless of the design, they all require a tight seal over the face so that the airway can be pressurized. This design requirement for a tight seal is the main limitation for making CPAP therapy more comfortable."
Oren says the VortexPAP eliminates the requirement for a tight seal since it's based on the reapplication of vortical airflow, a flow control mechanism commonly used in aerospace engineering applications.
"The unique aerodynamic properties of vortical airflow enable the device to pressurize the upper airways without needing a tight-fitting mask," says Oren. "As a result, this game-changing innovation will make CPAP therapy more comfortable and better tolerated and may increase patient compliance, a win for patients, doctors, and third-party payers. Over 40 million people in the U.S. are diagnosed with OSA, but the actual number is likely even higher because many remain undiagnosed."
The project is a collaboration between Oren; Roy Kulick, MD, UC Entrepreneur-in-Residence; Ephraim Gutmark, Ph.D., Distinguished Professor, Ohio Eminent Scholar in the UC Department of Aerospace Engineering; and Ann Romaker, MD, director of the UC Sleep Medicine Center and professor in the UC Department of Internal Medicine.
Gutmark is the director of the UC Laryngeal Biomechanics Lab. "The main strength of our lab is marrying advanced knowledge in aerospace with medicine," Oren says. "For example, we know that vortices emanating from a jet engine would generate sound that people perceive as a type of 'noise.' As such, there is much active research on eliminating these vortices to reduce the sound (noise) produced by the jet.
"Our lab takes this knowledge and tries to reverse it. We found that vortices form in the airway when our vocal cords vibrate when we speak."
Oren says it is well-established in aerospace engineering that vortex airflow has unique aerodynamic properties that are different from conventional, continuous airflow. This type of airflow is used in various applications, such as enhancing fuel mixing in combustion processes, improving convective cooling of electronic components, or as a flow control mechanism that reduces drag over a body (such as an airplane wing or a car).
The co-inventors and Oren realized the unique properties of vortex airflow could also be leveraged for CPAP therapy.
"The development work of the VortexPAP draws on the strengths that UC offers," Oren says. "This idea was born from distinguished departments (aerospace engineering and otolaryngology) and developed into a functional, suitable medical device using expertise in biomedical engineering."
"We collaborate with Dr. Ann Romaker, a sleep medicine doctor from UC, who helped us identify the main reasons for patient noncompliance with CPAP therapy and ensure our technology offers an alternative, effective solution."
Romaker says the biggest design change is the lack of a need for a seal. The interface will not be tight nor will it have to be enclosed, so people with a degree of claustrophobia will be much more comfortable, as well as everyone else.
"The lower pressures produced by this method will also decrease air swallowing, which can be uncomfortable for some CPAP users and, again, will be more comfortable," Romaker says.
According to Oren, the development work is also done with the goal of eventually commercializing the VortexPAP in the U.S. As such, they received strong support from the UC Venture Lab. They paired with Entrepreneur-in-Residence Kulick, who has been instrumental in helping build out a business plan for the VortexPAP.
Provided by University of Cincinnati