Scientists find a possible mechanism determining human pregnancy success
Many pregnancies fail early in human embryo development, with 40 to 60 percent of the losses occurring just prior to or during implantation, a process that is initiated on days six and seven post-fertilization, when the conceptus is a blastocyst, and which continues until the placenta is established a couple of weeks later. However, our understanding of the circumstances that lead to pregnancy failure—and conversely, what underpins success—is quite rudimentary. Without that knowledge, our ability to mitigate early pregnancy failure is limited.
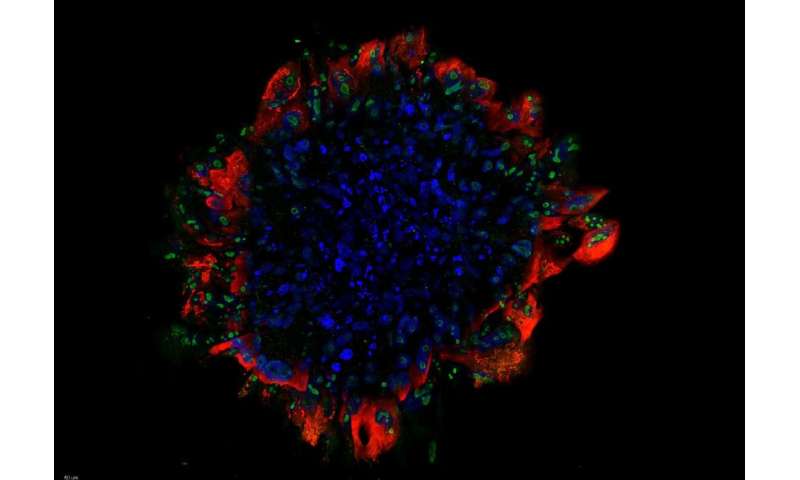
Using an extended culture system that allows conceptuses to continue in their development in vitro, Rachel West, Hao Ming, Deirdre Logsdon, and colleagues addressed this knowledge gap by performing single-cell RNA sequencing of human trophoblast (TB) cells that make up the early placenta on days eight, 10 and 12 after fertilization—a time corresponding to the first five days after the embryo begins to implant into the uterine wall. During this period, proliferating progenitor stem cells, called cytoTB (CTB) cells, gave rise to two distinct cell sub-lineages called syncytioTB (STB), which surround the conceptus, and migratoryTB (MTB) cells. STB cells expressed genes involved in producing placental hormones, which help to ensure successful continuation of the pregnancy. The motile MTB cells expressed genes that play a role in migration and invasion, and may facilitate implantation of the embryo into the uterine wall.
A surprising finding of this study is the high number of interferon receptors and some component effectors in the STB and MTB cells, suggesting that these cells are poised to respond to interferon. Interferon signaling has a well-known role in maternal recognition of pregnancy in ruminants, but little is known about its function in humans. Here, the scientists suggested that interferons released by the uterine cells may be able to trigger an interferon response in the early trophoblast and provide a first line of defense against pathogens and enhance embryo survival. This is in agreement with the observation that in vitro fertilization (IVF) patients with recurrent implantation failure have significantly lower levels of intrauterine interferon-gamma than normal pregnant women. On the other hand, excessive interferon exposure due to infection or inflammation could lead to desensitization of interferon pathways, block early trophoblast differentiation, and result in implantation failure. Therefore, interferon response may act as a safety switch that terminates the pregnancy to avoid further cost to the mother.
According to the authors, the findings may shed light on how the molecular cross-talk between the mother and early placental cells determines pregnancy success, and reveal mechanisms that facilitate human implantation. This study has made inroads toward understanding the underlying basis of an array of pregnancy disorders, including recurrent implantation failure, unexplained sporadic and recurrent pregnancy loss, and diseases of abnormal placentation. It provides an important step toward understanding these disorders and designing effective therapeutic interventions to improve implantation and pregnancy outcomes for IVF patients.
This story is part of Science X Dialog, where researchers can report findings from their published research articles. Visit this page for information about ScienceX Dialog and how to participate.
More information:
Rachel C. West et al. Dynamics of trophoblast differentiation in peri-implantation–stage human embryos, Proceedings of the National Academy of Sciences (2019). DOI: 10.1073/pnas.1911362116