Rethinking 'one appointment, one problem' for diabetes patients
I spent the majority of my life in the United States before relocating to the United Kingdom (UK) a few years ago. I quickly noticed the difference in primary healthcare structure. Healthcare in the U.K. is provided by the government-funded National Health Service (NHS). Patients are typically able to schedule an appointment or consultation the same day they inquire. However, these consultations are very short (less than 10 minutes). As a result, many General Practices (GPs) operate on a de facto "one consultation, one problem" policy.
Puzzlingly, I've found only a single mention of this policy in an opinion piece for the BMJ. The lack of public dialog is surprising, as both GPs I consulted as a patient at in the U.K. have had prominent and forceful signage to this effect. While a "one consultation, one problem" policy represents a minor annoyance to a generally healthy person, it got me thinking about people with more complex healthcare needs. As healthcare moves toward a holistic and personalized approach, I began to question whether the current system is antiquated.
My research focuses on improving patient care for people with type 2 diabetes mellitus (T2DM). T2DM patients require significant healthcare resources and are more likely to have other co-occurring chronic conditions, termed comorbidities. The common theme in my focus group of patients with T2DM was that they felt overwhelmed with the frequency of consultations when managing comorbidities on top of T2DM. In a recently published study, my colleagues and I describe consultations for people with T2DM and examine whether consultation rates, costs, and temporal trends during 2000–2018 differed by the number of comorbidities. The short answer is yes, but we had to look in more detail to develop a solution. For this study, we obtained primary care records for 120,409 adults with T2DM with an average of 5.6 years of post-T2DM-diagnosis consultation information for each patient. The number of prevalent and incident comorbidities were collected.
Consultation rate
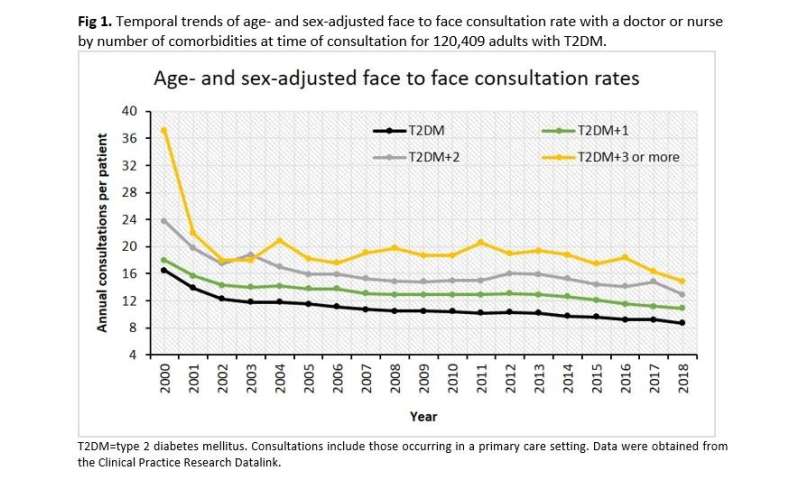
We found that patients with more comorbidities had more frequent consultations. For example, patients with T2DM only had a face-to-face consultation every 35 days, compared to every 20 days for patients with three or more comorbidities. This represents a large burden for patients with comorbidities who must take additional time away from their work and lives for frequent consultations. Frequent consultations also increase the chance that a consultation will be missed, interrupting the continuity of care. We further found that patients with more comorbidities were more likely to see a doctor than a nurse. This is more costly to the NHS per consultation, and in many cases, may be superfluous.
Consultation cost
In addition to the practical and mental burden on patients, there are also implications for the NHS. The annual consultation cost for a patient with three or more comorbidities is 1.9 times higher than that for a patient without comorbidities (£778.83 vs £412.70). This is due to an increase in both the frequency and likelihood of seeing a doctor rather than a nurse. It is important to note that the cost estimate does not include any tests, medications or secondary/tertiary care.
Temporal trend
The face-to-face consultation rate decreased, regardless of the number of comorbidities, from 2000-2018. We adjusted for sex and age to account for changing population demographics over time. Over nearly two decades, the adjusted rate change ranged from a maximum of -4.3% for three or more comorbidities to a minimum of -2.2% for two comorbidities. The reasons for the across-the-board decrease are not known. It is possible that fewer consultation slots are available, patients are having fewer emergent issues requiring a consultation, or consultations are occurring via another modality. Further research is necessary to understand this temporal change.
Consultation by telephone
While the rate of face-to-face consultations decreased, the rate of telephone consultations increased 51% during 2000–2018. Patients with three or more comorbidities had telephone consultations at three times the rate of patients without comorbidities. Day-to-day healthcare temporarily moved to non-face-to-face modes during the COVID-19 pandemic. I expect that we will see the popularity of telehealth continue to rise. In fact, telephone consultations may be a method to address both rising care cost and the patient burden, while ensuring patients are still able to consult with a healthcare professional.
The solution
Revising how patients with T2DM are managed is a cost-effective solution. This could involve a comprehensive, longer consultation once or twice yearly (either face-to-face or via telephone or video) where polypharmacy can be reviewed, patient education can be provided, and patients can have time to absorb the information and ask questions, supplemented by structured education programs (such as the Healthier You Diabetes Prevention Programme) and self-management apps. We believe this approach would reduce stress on patients, curb costs, and potentially result in better management of T2DM and comorbidities, leading to improved patient outcomes.
This is a great example of patient-involved research and using real-world data to address clinical questions. More information on this study can be found here: https://pubmed.ncbi.nlm.nih.gov/33539642/.
This story is part of Science X Dialog, where researchers can report findings from their published research articles. Visit this page for information about ScienceX Dialog and how to participate.
More information:
Briana Coles et al. Rates and estimated cost of primary care consultations in people diagnosed with type 2 diabetes and comorbidities: A retrospective analysis of 8.9 million consultations, Diabetes, Obesity and Metabolism (2021). DOI: 10.1111/dom.14340
Bio: Briana Coles is a Research Fellow in Epidemiology/Biostatistics with 10 years of research and research governance experience. Her research leverages complex real world datasets to improve clinical practice and patient outcomes. She is passionate about understanding the role of multimorbidity in health outcomes as well as factors that contribute to ethnic health disparities.